Diabetes is one of this century’s most significant global health emergencies, ranking among the ten leading causes of mortality and cardiovascular disease (CVD), respiratory disease, and cancer. According to the World Health Organization (WHO), non-communicable diseases (NCDs) accounted for 74% of deaths globally in 2019, of which Diabetes resulted in 1.6 million deaths, thus becoming the ninth leading cause of death globally.
[Data source WHO https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/ncd-mortality]

[Data Source ICMR https://main.icmr.nic.in/sites/default/files/upload_documents/ICMR_Guidelines_for_Management_of_Type_1_Diabetes.pdf]
Causes of Diabetes
- Multifactorial pathogenesis in which metabolic, behavioral, lifestyle and environmental factors precipitate disease in genetically predisposed persons
- The combination of insulin resistance increased hepatic gluconeogenesis, and relative defects in insulin secretion promote metabolic dysfunction.
- Overweight or obese body habitus is a significant factor contributing to insulin resistance, which is a precursor to glucose intolerance and diabetes development.
- A hypercaloric diet and sedentary lifestyle also worsen insulin resistance
- Hyperglycemia develops when progressive impairments in insulin secretion render pancreatic β-cells unable to maintain euglycemia
- Vital hereditary component contributes to the manifestation of the disease, with complex polygenic inheritance pattern underlying most cases
Risk factors of Diabetes
Age- Incidence increases with age, owing in part to age-related reduced glucose tolerance but also reduced physical activity and increased adiposity
- Polycystic ovary syndrome (PCOS)
- Delivery of an infant weighing more than 4 kg
- Previous diagnosis of gestational diabetes (Diabetes during pregnancy)
- Most cases of type 2 diabetes have a complex multifactorial polygenic basis, with over 100 loci identified as contributing to a higher risk.
- Genetic risk for type 2 diabetes is primarily expressed in environmental factors such as obesity and a sedentary lifestyle.
- Increased prevalence in African American, Latino, Native American, Pacific Islander, and Asian American populations
Other risk factors/associations
- Prediabetes (hemoglobin A1C level (HbA1C) 7%-6.4%; 5-fold elevated risk)
- Overweight or obesity (2-fold elevated risk if overweight; risk rises proportionately with a higher class of obesity)
- Sedentary lifestyle
- Medications that worsen glucose tolerance or exacerbate hyperglycemia, such as:
- GlucocorticoidsThiazide diuretics
- Atypical antipsychotics
- Sleep disorders (eg, obstructive sleep apnea, chronic sleep deprivation, night shift work schedule) in conjunction with glucose intolerance
What is Type 1 Diabetes?
Type 1 diabetes (previously known as insulin-dependent, juvenile, or childhood-onset) is characterized by low insulin production and requires daily administration of insulin. In 2017 there were 9 million people with type 1 diabetes; most of them live in high-income countries. Neither its cause nor the means to prevent it are known. Symptoms include excessive excretion of urine (polyuria), thirst (polydipsia), constant hunger, weight loss, vision changes, and fatigue. These symptoms may occur suddenly.What is type 2 Diabetes?
Type 2 diabetes (formerly called non-insulin-dependent or adult-onset) results from the body’s ineffective use of insulin. More than 95% of people with Diabetes have type 2 diabetes. This type of Diabetes is primarily the result of excess body weight and physical inactivity. Symptoms may be similar to type 1 diabetes but are often less marked. As a result, the disease may be diagnosed several years after onset, after complications have already arisen. Until recently, this type of Diabetes was seen only in adults, but it is now also occurring increasingly frequently in children.Prevention
Simple lifestyle measures are effective in preventing or delaying the onset of type 2 diabetes. To help prevent type 2 diabetes and its complications, people should:- Achieve and maintain healthy body weight;
- Be physically active – doing at least 30 minutes of regular, moderate-intensity activity on most days. More activity is required for weight control;
- Eat a healthy diet, avoid sugar and saturated fats; and
- Avoid tobacco use – smoking increases the risk of Diabetes and cardiovascular disease.
Diagnosis and treatment
- Early diagnosis can be accomplished through relatively inexpensive testing of blood sugar.
- Treatment of Diabetes involves diet and physical activity along with lowering blood glucose and the levels of other known risk factors that damage blood vessels. Tobacco use cessation is also important to avoid complications.
- Interventions that are both cost-saving and feasible in low- and middle-income countries include blood glucose control, particularly in type 1 diabetes. People with type 1 diabetes require insulin. People with type 2 diabetes can be treated with oral medication but may also require insulin, blood pressure control, and foot care (patient self-care by maintaining foot hygiene; wearing appropriate footwear; seeking professional care for ulcer management; and regular examination of feet by health professionals).
Intelehealth and MSF India Response
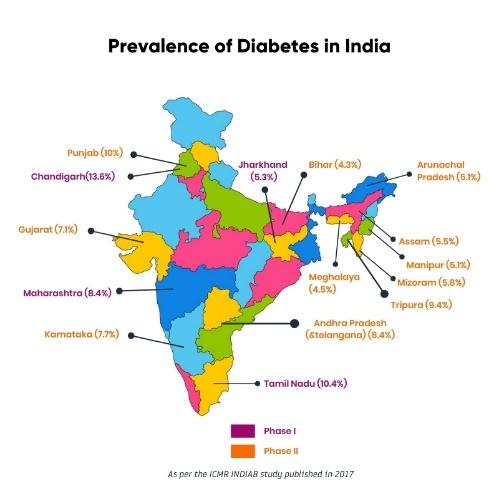
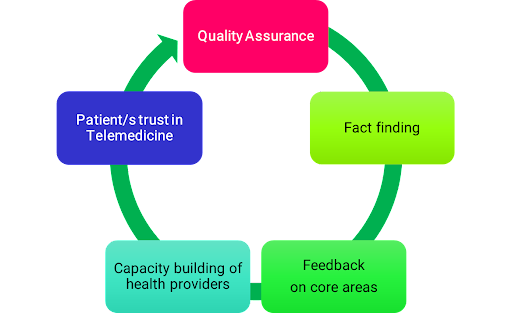
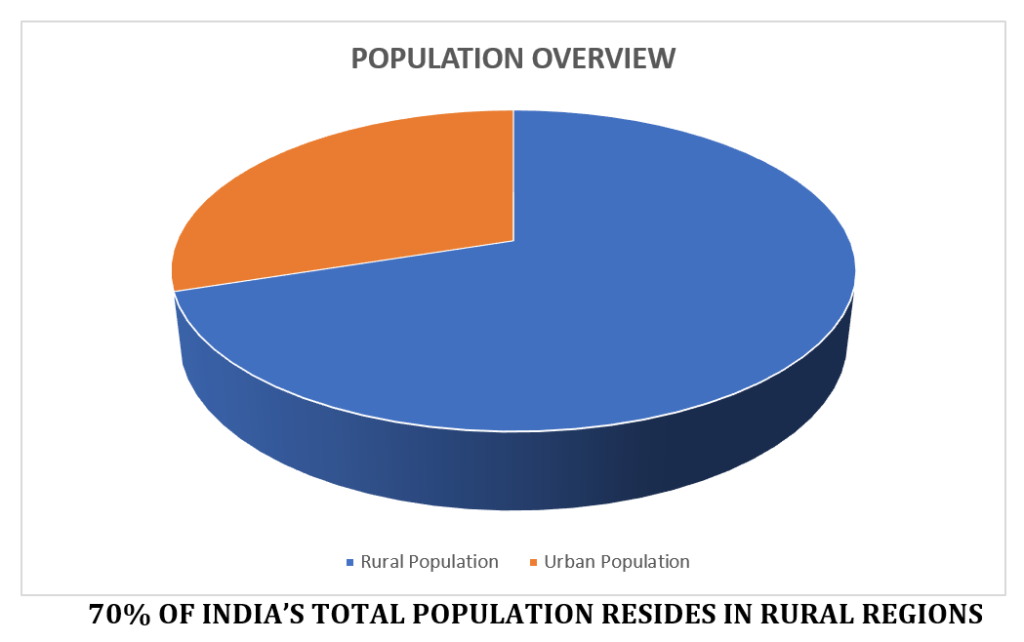
Diabetes is rising in India, with the second-highest diabetics due to increased sedentary lifestyles, unhealthy diets, tobacco use, and obesity. Nearly 50% of the population are unaware that they have Diabetes. Intimidated by the stats showing India has the second highest number of diabetics in the world, MSF India launched the telemedicine Diabetic Management Helpline, powered by Intelehealth, to provide primary-level diabetes care and manage the disease and encourage healthy living. A pan-India toll-free helpline would improve access to standardized and uniform helpful information about diabetes care which would be customized to their needs. This would significantly help the underprivileged, who would otherwise postpone or even forgo needed healthcare due to non-affordability. Such digital technology platforms motivate the patients for diabetes self-management through constant follow-ups, counseling and access to a diet plan. The helpline would allow the patients to seek consultations at their convenience. By providing appropriate counseling on healthy meal plans and lifestyle modifications by an accredited dietician, increasing awareness, and promoting self-monitoring of health and routine follow-ups, the helpline could minimize the risks of future complications. Additionally, the helpline would also support the patients in seeking psychological healthcare, which is crucial to the overall management of Diabetes, without the fear of stigmatization. If you have Diabetes and need medical assistance, contact the Diabetic Management Helpline. Call 1800 309 4144 and connect with a team of nurses, doctors & nutritionists and learn how to manage your diabetes effectively.

References:
1. Dluhy RG et al: Intensive glycemic control in the ACCORD and ADVANCE trials. N Engl J Med. 358(24):2630-3, 2008
2. Tancredi M et al: Excess mortality among persons with type 2 diabetes. N Engl J Med. 373(18):1720-32, 2015
3. Skyler JS et al: Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA Diabetes Trials: a position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. J Am Coll Cardiol. 53(3):298-304, 2009
4. Riddle MC et al: Consensus report: definition and interpretation of remission in type 2 diabetes. Diabetes Care. ePub, 2021
5. Nathan DM: Diabetes: advances in diagnosis and treatment. JAMA. 314(10):1052-62, 2015
6. Bonnefond A et al: Rare and common genetic events in type 2 diabetes: what should biologists know? Cell Metab. 21(3):357-68, 2015
7. American Diabetes Association Professional Practice Committee et al: 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes-2022. Diabetes Care. 45(Supplement_1):S17-38, 2022
8. Selvin E et al: Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 362(9):800-11, 2010
9. Nguyen NT et al: Relationship between obesity and diabetes in a US adult population: findings from the National Health and Nutrition Examination Survey, 1999-2006. Obes Surg. 21(3):351-5, 2011
10. Telemedicine Cost–Effectiveness for Diabetes Management: A Systematic Review:Jun Yang Lee and Shaun Wen Huey Lee
11. Telemedicine Application in the Care of Diabetes Patients: Systematic Review and Meta-Analysis : Milena Soriano Marcolino, Junia Xavier Maia, Maria Beatriz Moreira Alkmim, Eric Boersma, Antonio Luiz Ribeiro






















 Health worker Minj(white coat) at Khusboo’s house during her home to home visit
Health worker Minj(white coat) at Khusboo’s house during her home to home visit


 Dr. Raghunandan Mehta – National President, Ekal Arogya Yojana (AFI) & Volunteer Doctor, Ekal Arogya Hepline
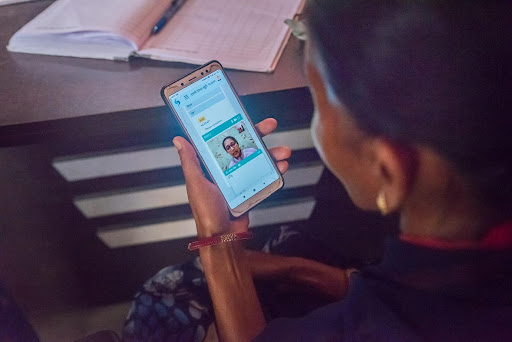
Dr. Raghunandan Mehta – National President, Ekal Arogya Yojana (AFI) & Volunteer Doctor, Ekal Arogya Hepline Dr. Mehta tele-consulting patients via Ekal Arogya Helpline
Dr. Mehta tele-consulting patients via Ekal Arogya Helpline




 Shamina spreading awareness about Vikalp Helpline in Udaipur
Shamina spreading awareness about Vikalp Helpline in Udaipur