Author – Dr Nalanda Singh (Medical Consultant, Intelehealth)
The draft document has been released in the public domain recently by National Medical Commission (NMC) regarding Professional Conduct Regulations (2022) which includes Telemedicine Practice Guidelines for Registered Medical Practitioners (RMP). This will serve as a set of self-regulatory guidelines for the RMP to practice medicine both physical and remote teleconsultations, and commitment to patients, society, and professional colleagues.

Highlights:
Prefix, Suffix, and Modern Medicine:
Only those RMPs who are registered under NMC Act, 2019, can use Medical
Doctor (Med Dr.) as a prefix before their names
Only NMC recognized medical degree/ diploma as a suffix
All RMPs, employed or self-employed should display the unique registration number below the RMPs’ signatures
RMPs are allowed to practice only one system of medicine.
RMPs need to be involved in public education & awareness activities without involving advertisement.
Prescribing Generic Medicine:
Every RMP is expected to prescribe drugs using “generic”/“non-proprietary”/“pharmacological” names only.
Encourage patients to purchase drugs from Jan Aushadhi Kendras.
To avoid misinterpretation prescriptions should preferably be written in capital/ typed and printed.
Continuing Professional Development (CPD):
30 credit hours required every 5 years, to be updated online regularly by
receiving training from recognized medical colleges, health institutions or medical societies.

Ethics:
Guidelines reflect relevant professional as well as social expectations from
RMP.
Must not refuse to treat a patient in case of a medical emergency, nor
discriminate based on gender, religion, caste, or economic grounds.
In case of abusive, unruly violent patients or relatives, the RMP can document, report, and refer the patient.
When an epidemic occurs, an RMP with all necessary medical protection and his own health permitting should not abandon his/her duty for the fear of contracting the disease him/herself.
Should not engage in endorsement or promotion of any drug, or medical product.
RMP & their families must not receive any gifts/travel facilities/ hospitality /cash/ monetary grants.
Inclusion of Declaration of Geneva 2017 called ‘The Physician’s Pledge’.
Penalties:
Strict and detailed penalties have been enumerated for uniformity across the country in the assessment of liabilities and award of disciplinary actions in case of professional misconduct.
The disciplinary actions mentioned are – Reformation, Temporary suspension of license to practice, which can range from 1 month to 3 years.
Debarring the RMP will depend on the level (severity) of misconduct proved.
Digitization of Medical Records:
Every self-employed RMP shall maintain medical records of all patients for 3 years from the date of the last contact with the patient. This should be done within 3 years of publication of the official gazette.

Consent:
Before performing any clinical procedure, or operation, the RMP should obtain the documented informed consent of the patient. In case the patient is unable to give consent, the consent of the legal guardian or family member must be taken.
In an operation that may result in sterility, the consent of both husband and wife is required.
In-vitro fertilization or artificial insemination shall be undertaken only after informed written consent from the female patient, spouse, and the donor.
A RMP shall not publish photographs or case reports of patients without their permission in a manner by which their identity could be revealed.
For the use of patient data in academic teaching or clinical case discussions, patient consent is required. Under no circumstances will the patient’s data be posted on social media.

Social media conduct:
RMP can provide factually verified information/ announcements on social media.
Should avoid discussing treatment or prescribing medicines and soliciting patients on social media
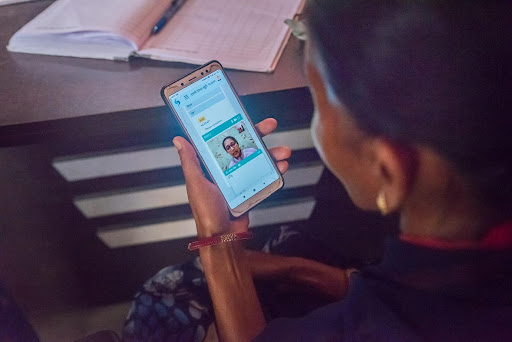
Telemedicine:
Principles of medical ethics that are mandatory for the profession must also be respected in the practice of telemedicine.
A RMP is eligible to provide telemedicine consultations from any part of India and should be familiar with guidelines, processes, and limitations of telemedicine practice, hence they need to undergo CPD training on the same.
Teleconsultations should not be anonymous, the patient and RMP should know each other’s identities.
In the case of a minor patient, teleconsultation should proceed only in the presence of a parent/legal guardian.
Patient confidentiality, privacy, and data integrity should not be compromised.
Mandatory consent.
Telemedicine Application types-
Mode of communication – video, audio, text
Timing of the information transmitted – real-time, asynchronous
Purpose of the consultation – nonemergency (first consultation & follow up), emergency (first aid, counseling, referral)
Interaction between individuals involved – patient to RMP, caregiver to RMP, RMP to RMP, health worker to RMP.
Patient management-
Health education- related to health promotion & prevention
Counseling- specific advice related to underlying condition
Medicines- can prescribe any drug except schedule X drugs
Guidelines for technology platforms enabling telemedicine:
RMPs must not participate in telemedicine platforms that provide ratings by the patient or others including reviews, advertisements, and promotions of RMPs by any means (manipulation of algorithms/search engines).
Technology platforms providing telemedicine services are obligated to ensure that consulting RMPs are duly registered.
The platform must provide the name, qualifications, registration number, and contact details of every RMP.
In case of non-compliance with guidelines/ existing laws applicable to the
provision of services, appropriate legal action can be initiated against the
platform.
Artificial intelligence/ machine learning is not allowed to counsel the patients or prescribe any drugs but can assist and support the RMP on
evaluation, diagnosis, or management.
Technology platforms must ensure a proper grievance redressal mechanism for end-users of their services.



