Authors: Dr. Srilekha C., Medical Consultant
The Shift in Maternal Care

Over a few decades, women are constantly encouraged to give birth in health care facilities so they may have access to skilled health care professionals and should the need for additional care arise the measures can be taken. However, accessing skilled and professional care in health facilities may not completely guarantee respectful, good, and quality care. Every woman has the right to have a positive and pleasant childbirth experience with Quality care. Ideally the expected quality care includes respectful care of the woman in labour, good and respectful communication, and making sure she feels emotionally and socially supported in the way that she desires.
Worldwide, maternal health efforts are shifting from an emphasis on boosting service utilization to improving quality of care. This change has been accompanied by a growing body of work on how women are treated during facility-based childbirth, which was first brought to global attention in 2010 by Bowser and Hill’s landscape analysis. This chilling quote from the report highlights how women may experience physical abuse during labour.
“When a woman goes into the second stage of delivery, you don’t want her to close her legs, so you’re beating her” [Kenya] (Center for Reproductive Rights & Federation of Women Lawyers–Kenya (FIDA), 2007)
Respectful maternity care (RMC) provides meaningful experiences of childbirth as a basic element of quality health, which includes knowing their self-worth, feelings, and preferences. RMC is globally recognized. Every woman around the world has a right to receive respectful maternity care. The concept of “respectful maternity care” has evolved and expanded over the past few decades to include diverse perspectives and frameworks. Advocates emphasized the need to humanize birth, taking a more holistic approach.
What it takes
Respectful maternity care (RMC) is not only a crucial component of quality of care; it is a human right. In 2014, WHO released a statement calling for the prevention and elimination of disrespect and abuse during childbirth, stating that “every woman has the right to the highest attainable standard of health, including the right to dignified, respectful care during pregnancy and childbirth.”WHO also called for the mobilization of governments, programmers, researchers, advocates, and communities to support RMC. In 2016, WHO published new guidelines for improving quality of care for mothers and new-borns in healthcare facilities, which included an increased focus on respect and preservation of dignity. In addition to the eight domains of quality of care, the framework also includes six strategic areas to help build a systematic, evidence-based approach for providing quality care: Clinical guidelines, Standards of care, Effective interventions, Quality measures, and Relevant research and capability building.
The ‘Holistic Way’
RMC is an approach centered on the individual, based on principles of ethics and respect for human rights, and promotes practices that recognize women’s preferences and women’s and new-borns’ needs.
Understanding a woman’s perspective and her needs during childbirth and addressing them as part of quality-improvement programmes can make delivery care safe, affordable, and respectful. The patient’s judgement on the quality and goodness of care is indispensable to improving the management of healthcare systems.
Respectful Maternal Care (RMC) is defined as “care organized for, and provided to all women in a manner that maintains their dignity, privacy and confidentiality, ensures freedom from harm and mistreatment and enables informed choice and continuous support during labor and childbirth.”
The Real Plight
It is a human right for every woman to deserve respectful maternity care, yet many women abstain from obtaining professional maternity care due to the lack of respect and being abused during labour. As per research and reports this leads to birth injury, and maternal and new-born deaths. Despite such severe impacts, these issues remain under wraps and especially so in developing nations.
Disrespectful and undignified care is prevalent in many facility settings in India, particularly for underprivileged populations, and this not only violates their human rights but is also a significant barrier to accessing intrapartum care services.
Bowser and Hill categorized disrespect and Abuse (D&A) faced by pregnant women into seven major categories – physical abuse, they are non-consented clinical care, non-confidential care, non-dignified care (including verbal abuse), discrimination based on specific patient attributes, abandonment, denial of care, and detention in facilities.
Improving the quality of health–care services by providing respectful maternity care (RMC) could lead to further reduction in Maternal mortality rate (MMR). Adopting a patient–centric approach and training of providers focused on respectful care would significantly improve the quality of care, promote institutional births, and protect the fundamental right of women to equity, dignity, and respect.
A Pathway Towards Respectful Maternity Care…
Several studies have documented the ubiquitous nature of disrespectful care and its adverse effects on care-seeking behaviour, and calls to action on quality of maternal health care have prioritised women’s experiences.
The findings from a study with an objective to estimate the prevalence of Disrespect and Abuse (D&A) and its determinants during pregnancy, childbirth, and immediate postpartum period among women in India provide crucial information to widen the scope of research on the effects of socioeconomic status on Respectful Maternal Care.
A study was conducted at Jamtara district in Jharkhand, with an objective to understand the aspects of care that women consider important during childbirth6\. Jharkhand is a state in eastern India with poor maternal and child health indicators.
Aspects of care most cited by women to be important in facility-based childbirth were – the availability of health providers and appropriate medical care (primarily drugs) in case of complications, emotional support, privacy, clean place after delivery, availability of transport to reach the institution, monetary incentives that exceed expenses, and prompt care. While some other factors include kind interpersonal behaviour, cognitive support, faith in the provider’s competence, and overall cleanliness of the facility and delivery room.
A low cost RMC-promoting interventions recommended by the WHO is the presence of a birth companion during labour and delivery. A birth companion is not only a key component to fulfil the objective of RMC, but, is also vital in improving the quality of care during labour and delivery.
Presence of a Birth companion during labour in a labour ward usually was not a regular practice in the past, hence there was an unmet need to implement this initiative to improve the quality of maternity care and to ensure a positive pregnancy outcome for every woman. Despite the known benefits, allowing birth companions is not in practice in government set-ups and in most private healthcare facilities in India. There is also a dearth of literature focusing on the method of implementation of a birth companion, which is a major challenge in busy labour and delivery wards.
A study was conducted in the Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, New Delhi with the objective to establish a practice of allowing a companion during labour and delivery. It followed the principles of Quality Improvement (QI), which included analysis of the problem and implementation of Plan-Do-Study-Act (PDSA) cycles for a step-by-step approach to provide quality care. A QI team was formed, and after obtaining the baseline data, problems were analysed using fish bone chart. A new policy of allowing birth companion was made and efforts made to sensitise and train the doctors and nurses posted in labour ward.
Simple interventions such as dress code for birth companions, curtains for ensuring privacy, display of posters and frequent reminders on WhatsApp groups were planned. The results of the study were the median value of women accompanied by birth companion marginally increased to 25% after the first PDSA cycle. Implementation of further changed ideas led to increase in median, which reached 66.6%. Thereafter, there was a decline, but by the end of 6 months, it was possible to attain the goal to establish a practice of allowing a companion during labour and delivery by using the principles of quality improvement (QI)and sustain it.
The findings revealed a direct relationship between respectful maternity care and positive childbirth experience7. Therefore, it is recommended that mangers and policy makers in childbirth facilities reinforce facilitating respectful maternity care to improve women’s child birth experience and prevent potential adverse effects of negative childbirth experiences.
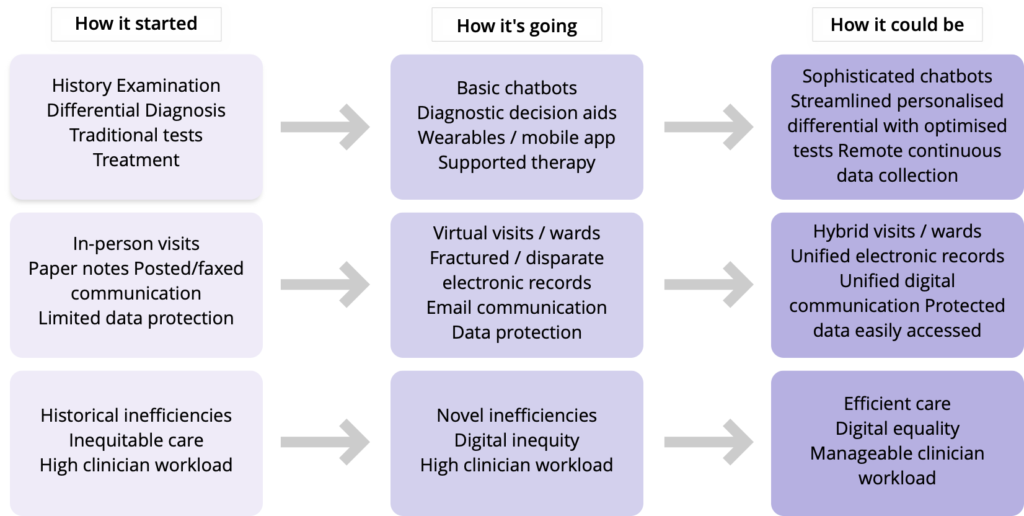
A simple tool that standardizes and measures whether best practices in RMC are being followed in the labour ward is the new WHO Labour Care Guide. The Labour Care Guide replaces the WHO partograph. It places an importance on not just adherence to process, but also the quality of the service delivery and person-centered care.
Intelehealth along with several clinical partners is working on a digital health solution, called eZazi, that adapts the WHO Labour Care Guide to a digital tool with integrated telemedicine support to improve the quality of care delivered in labour wards. This new product is another step towards achieving our vision of ethical, evidence-based and dignified healthcare for every woman.
The Need of the Hour
Raising awareness and strengthening the capacity of the interested parties regarding concepts and practices related to respectful maternity and new-born care; identifying the legal frameworks which support it; recognizing and describing the use of some of these tools to plan, implement and monitor quality improvement initiatives for maternity and new-born care in health care services.
The need of the hour is collaboration and investment that include diverse donors, partners, and experts with an interest in RMC for a sizeable impact.

https://www.who.int/news/item/15-12-2020-monitoring-childbirth-in-a-new-era-for-maternal-health