Author : Dr. Shilpa Bhatte (Chief Program Officer – Global Lead, Intelehealth)
Telemedicine is the remote diagnosis and treatment of patients using telecommunications technology.
It is a reasonably new medium for providing and seeking healthcare services due to its sudden thrust into the limelight during the COVID-19 pandemic. As healthcare providers, we are still in the process of understanding and exploring how these services can be optimized and made effective and efficient to suit patients’ needs while also inculcating a sense of trust in the medium through which the advice is provided.
At Intelehealth, we believe that healthcare providers will need ongoing user support and troubleshooting with tech-related issues to adapt to a new medium and will require support to deliver healthcare advice effectively.
To support our healthcare providers and standardize their skills – we maintain a rigorous quality assurance mechanism for our helplines and telemedicine platforms. Specifically, with helplines, we do a thorough and ongoing medical audit of a few core areas, such as:
- Communication skills
- Quality of the advice/information provided
The clinical team conducts the audit based on details recorded on the app and given to them. But they can contact the concerned backend doctor/s, frontline health worker/s, or patient/s for further understanding.
With communication skills, our focus is to emphasize the need to engage the patients with empathy and compassion, understand their symptoms and ask relevant questions to understand the morbidity better.
- Introduction: Stating who you are and the organization/government you are calling on behalf of is extremely important, along with the reason for the call – it can be disorienting to a person/patient if they do not understand who you are and the nature of the call
- Using speech effectively: Speaking slowly is essential, and so is pronouncing words well. Maintaining a calm tone is important, and mumbling or speaking fast may have a counter-effect in the person not being interested in the consultation. One has to also quickly assess if they can hear your questions satisfactorily and can respond accordingly.
- Language: It is essential to adjust the language according to the listener/patient, optimizing their engagement and responses. It is also vital to always be respectful and empathetic in your questions
- Minimize use of medical language: Health providers assume that patients will understand the nature of the morbidity under question. This may not always be true. Hence use descriptive language to explain the color, shape, size, etc.
- Script: Having a written down prompt sheet is extremely important to ensure all the points that need to be covered are completed. This ensures that the call was efficient in receiving information from the patient in case the conversation drifts and hence helps bring back focus to the subject under scrutiny.
- Listen well: Communication is about speaking and active listening, which shows the person/patient that you are paying attention to what they are saying.
- Summarizing: Repeating important information/instructions on prescription helps ensure that the advice provided was well received and understood. Note down a follow-up schedule if required or pertinent
While assessing the quality of advice/information provided by the health provider, our focus is to evaluate:
- Ensure that evidence-based information is provided to the patients
- Updated information based on local government guidelines is provided
- Wherever possible – holistic information on preventative, curative, and/or treatment plans is shared with patients
- Treatment standards are applied to ensure that all patients receive appropriate care regardless of financial means
Overall the Medical audit includes the vetting of the following parameters:
- Registration: Process, Completeness, Closure of visit
- Demographic details
- Consent
- Case history: Completeness of information by matching with an appropriate mind map and checking for ambiguity in the information given in the recording versus that registered on the app
- Issues about past, family history, etc
- Issues about measuring and registering vitals: Registering vitals, the correctness of values
- Issues about physical examination including complete assessment: Diagnosis, investigations, prescription, follow-up, referral
- Turnaround time – TAT: time-lapse between upload of the case and a prescription issued
- Time-lapse between consultation by backend doctors and patients receiving prescription
- Patient outcome
- Tech-related issues: app or user-related issues
- Doctor patient communication
- Quality of advice and information provided
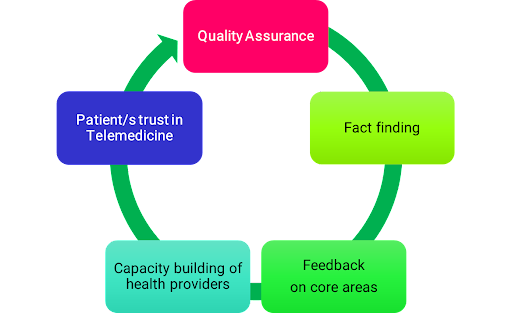
The quality assurance process is a fact-finding process rather than a fault-finding endeavor to provide regular feedback to the health providers to build their capacity to provide effective and efficient teleconsultations. This, in turn, has a virtuous effect on the trust-building process between patients and telehealth providers and increases the robustness of the telemedicine platform.

Dr. Gulhan Abdullaevna at Razzakov city headquarters checking the doctors web page at Batken, Kyrgyzstan

Renu Kumari, Community Health Officer using eSanjeevani app at Dorma Health & Wellness Centre, Khunti district, Jharkhand