In today’s rapidly evolving healthcare landscape, telemedicine is revolutionizing how medical services are delivered. From remote patient monitoring to AI-driven diagnostics, telehealth technologies are bridging gaps in healthcare accessibility and efficiency. Whether you’re a healthcare provider, policymaker, or digital health enthusiast, understanding key telemedicine terms is essential. This glossary provides a structured reference for the most important telemedicine-related terminology.
1. Broad Terms in Digital Health
The field of digital health encompasses a wide range of technologies and services:
- Telehealth – A broad term referring to the use of digital and telecommunication technologies to deliver healthcare services remotely. It includes both clinical (telemedicine) and non-clinical services such as health education, administrative meetings, and remote monitoring.
- Telemedicine – A subset of telehealth that focuses specifically on the remote delivery of clinical medical services, such as diagnosis, treatment, and follow-up consultations by licensed healthcare professionals
- eHealth – The use of digital tools and electronic communication in healthcare.
- mHealth (Mobile Health) – Healthcare delivery through mobile devices, applications, and wearable sensors.
- Connected Health – Integration of technology to create seamless healthcare experiences across multiple platforms.
- Health Informatics – The application of information technology to healthcare for data management and decision support.
2. Service Delivery Modes
Telemedicine services can be delivered in various ways to meet different patient needs:
- Teleconsultation/Teleconsult/Virtual Visit – Remote consultation between a healthcare provider and a patient.
- Teletriage – Remote assessment of symptoms to determine urgency and level of care needed.
- Telemonitoring / Remote Patient Monitoring (RPM) – Continuous monitoring of patient health data remotely using digital devices.
- Telecare – Remote support services, particularly for elderly or chronically ill patients to support care at home
- Tele-expertise – Specialist-to-specialist consultations and knowledge sharing.
- Telementoring – Remote guidance from experts to healthcare providers in training or in low-resource settings.
- Telecoaching – Digital coaching for lifestyle changes and chronic disease management.
- Tele-advice – Non-clinical medical guidance, often used for second opinions.
- Telefollow-up – Remote post-treatment monitoring and check-ups.
- Tele-intervention – Remote healthcare procedures or immediate intervention for acute conditions.
3. Specialty-Specific Telemedicine
Different medical specialties have embraced telemedicine to provide specialized care remotely:
- Telepsychiatry – Remote mental health consultations and therapy.
- Teledermatology – Remote diagnosis and treatment of skin conditions.
- Teleradiology – Remote analysis of radiology images such as X-rays, CT scans, and MRIs.
- Telecardiology – Remote diagnosis and management of cardiovascular conditions.
- Teleoncology – Remote cancer care, consultation, and treatment planning.
- Telepediatrics – Remote pediatric consultations and care for children.
- Telegeriatrics – Remote care services tailored to elderly patients.
- Teleophthalmology – Remote diagnosis and management of eye diseases and vision care.
- Teledentistry – Remote dental consultations and oral health assessments.
- Telepharmacy – Remote prescription services and medication management.
- Teleorthopedics – Remote musculoskeletal and orthopedic care.
- Teleobstetrics – Remote prenatal and maternal health monitoring.
- Tele-endocrinology – Remote management of diabetes and hormonal disorders.
- Telepathology – Remote pathology services, including digital biopsy analysis.
- Tele-ICU – Remote intensive care unit monitoring and critical care support.
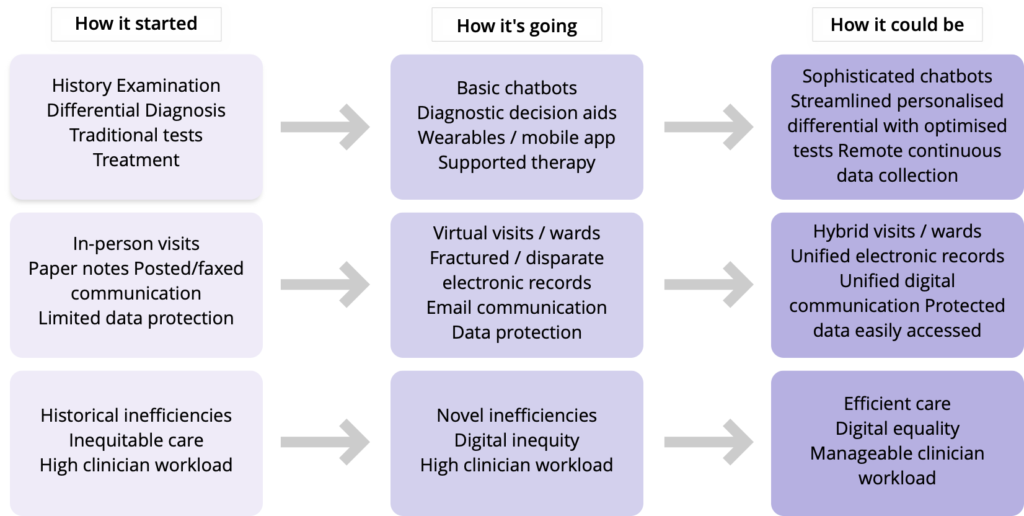
4. Telemedicine Technologies
Innovative technologies enable telemedicine to deliver high-quality care remotely:
- Asynchronous/Store-and-Forward Telemedicine – Sending patient data (e.g., images, reports) for later review by a specialist.
- Synchronous/Real-Time Telemedicine – Live video consultations between patients and doctors.
- AI-Assisted Telemedicine – Use of artificial intelligence to support diagnosis, triage, and decision-making.
- Wearable Health Technology – Devices that monitor patient vitals and transmit data remotely.
- Telepresence – Use of robotics or smart devices to enable a healthcare provider’s remote presence in a clinical setting.
5. Healthcare System & Policy Terms
The implementation of telemedicine requires robust healthcare policies and systems. These terms are often used in the context of implementing telemedicine in the health system.
- Telehealth Infrastructure – Digital platforms, networks, and policies supporting telemedicine services.
- Interoperability in Telehealth – The seamless integration of electronic health records (EHRs) and digital health platforms.
- Digital Therapeutics (DTx) – Evidence-based digital health interventions designed to prevent, manage, or treat diseases.
- ePrescribing (eRx) – Digital prescription services allowing healthcare providers to send prescriptions electronically.
- Digital Public Health – The use of digital technologies in population health and disease prevention efforts.
- Remote Health Management (RHM) – Strategies for delivering remote healthcare services at scale, often for chronic disease management.
Conclusion
Telemedicine is transforming healthcare by making it more accessible, efficient, and patient-centered. As these technologies continue to evolve, staying informed about key terminologies will help stakeholders navigate this rapidly changing field. Whether you’re a healthcare provider, a digital health entrepreneur, or a policymaker, understanding telemedicine terms is the first step toward leveraging these innovations for better healthcare delivery.
Let us know if there are any other telemedicine-related terms you’d like to see in this glossary!



 What if one could save 2 million lives globally by investing as little as US$ 0.24 per patient per year?
What if one could save 2 million lives globally by investing as little as US$ 0.24 per patient per year?