 What if one could save 2 million lives globally by investing as little as US$ 0.24 per patient per year?
What if one could save 2 million lives globally by investing as little as US$ 0.24 per patient per year?
Wouldn’t that be a great investment? The WHO report- “Going digital for noncommunicable diseases” shows exactly such a pathway. Noncommunicable diseases (NCDs), particularly cardiovascular diseases, cancers, diabetes and chronic respiratory diseases, are responsible for 74% of deaths globally and negatively impact the lives of millions more. Here are some of the key takeaways from the report:
1. Digital Health’s Role in Addressing NCDs: Telemedicine is particularly well-suited for managing chronic diseases, which require continuous monitoring and long-term care.Digital health technologies, including telemedicine, mobile apps, and chatbots, offer innovative ways to improve prevention, management, and treatment of NCDs.
2. Telemedicine: A Game-Changer for Remote Care: Currently one of the biggest challenges facing the public healthcare system is the sheer cost of building and supporting infrastructure to provide care for rural and underserved communities. Telemedicine allows for remote teleconsultations and continuous monitoring of chronic conditions, reducing the need for hospital visits. One is able to offer real-time care and improved decision-making without any additional time and money spent on travel and other logistical arrangements at the patient’s end.
Key Findings from the WHO Report |
3. Cost-Effective Solutions with High Returns on Healthcare Outcomes: A minimal investment of US $ 0.24 per patient annually in digital tools could save over 2 million lives and bring US $199 billion in economic benefits by 2033. There is a return on investment of 19 US $ on every US $ invested. Telemedicine reduces hospitalisation rates and long-term healthcare costs, making it a highly cost-effective solution.
4.Barriers and Challenges in implementing Telemedicine: Some key barriers include inadequate digital infrastructure in low-resource settings, limited digital literacy (in both patients and healthcare providers), and concerns over data privacy and regulation. To overcome these, one needs to invest in a variety of digital health technologies, train healthcare providers as well as individuals located within communities, and shape the right kind of digital governance policies and structure to ensure equitable access to digital healthcare.
5. The Future of Healthcare is Digital: Digital health has transformative potential for achieving universal health coverage. Telemedicine, as part of a broader digital health ecosystem, holds the promise of transforming healthcare delivery, making it more inclusive, efficient, and patient-centered. Its potential to improve NCD outcomes, particularly in underserved populations, makes it an indispensable tool for the future of global health.
You can access some notable case studies in the report. The document can be accessed here.
Intelehealth will be working with the task force at WHO to help turn this vision into a reality. We are committed to helping build an ecosystem that provides healthcare to the widest possible cross-section of underserved populations across geographies.



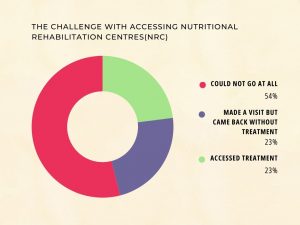
 Intelehealth’s study in Nashik District aims to tackle Severe Acute Malnutrition (SAM) through an innovative app-based plan.
Intelehealth’s study in Nashik District aims to tackle Severe Acute Malnutrition (SAM) through an innovative app-based plan.